The Principle of Autonomy – Does it Support the Legalisation of Euthanasia and Assisted Suicide (Dr Xavier Symons)
Read in PDFThe principle of autonomy is often invoked in support of the legalisation of euthanasia and assisted suicide. How one defines ‘autonomy’, however, is a matter of dispute. A number of important considerations arise as a result of this dispute, and it is important to ensure that ‘autonomy’ is defined in a way that works for the common good.
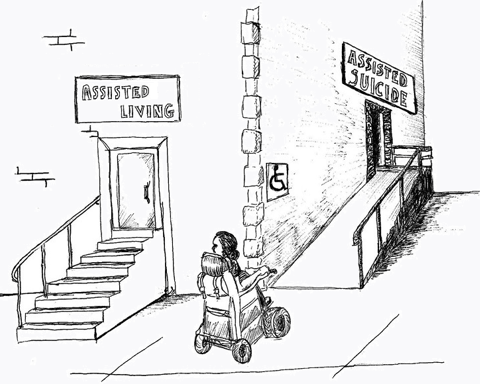
Two definitions frequently offered draw upon ‘informed consent’, on the one hand, and ‘self-definition’, on the other. Exploring the constituent elements of these definitions shows that euthanasia and assisted suicide diminish rather than affirm the autonomy of patients.
In addition to this diminishment, the social bonds which guarantee the common good are weakened. This occurs because definitions of autonomy which lend support to euthanasia and assisted suicide require the lifting of limits normally set on autonomy. Other aspects of life are, however, uncontroversially subject to such limits, and so it is inconsistent to efface them in the deployment of an understanding of autonomy that justifies euthanasia and assisted suicide.
What is required instead is an understanding of autonomy which does not eclipse a connection to the common good. This begins with a recognition of the social nature of human life: how an individual life always affects the life held in common by society, and how our dependence on others is fundamental in our understanding of the human person.
Euthanasia and assisted suicide are in fact hindrances to the exercise of authentic autonomy, not its realisation in the face of difficulty.
It is commonplace in liberal democratic societies to extol the importance of personal autonomy. But what exactly does it mean to respect autonomy? Many people believe that respect for autonomy requires the removal of all constraints on one’s capacity for self-determination and self-expression. This briefing paper, however, argues that an adequate conception of autonomy ought to be set against the backdrop of an objective moral order and situated in the context of the common good. Autonomy ought to be conceived of as part of a matrix of social conditions that taken together are conducive to the realisation of basic human goods. Autonomy is one condition, but not the only condition, for human flourishing. Or, as Daniel Sulmasy has written, “free choice is the context of morality, not the content of morality”. Autonomous choices should be aimed at basic goods – or, at least, not be in violation of basic goods – for such choices to be considered authentic exercises of autonomy.
The exercise of authentic autonomy, furthermore, is enabled by virtue of the human communities to which one belongs. Human beings become mature practical reasoners through education and life experience, and both these come from the communities of which one is a part – the family, friendships, neighbourhoods, educational institutions, intellectual communities, clubs and societies, religious tradition(s), and so forth. As such, respect for autonomy requires that we seek to preserve and sustain the community norms and relationships that enable authentic expressions of autonomy.
Such a conception of autonomy draws attention to the social harms attendant to the legalisation of euthanasia and assisted suicide. The legalisation of euthanasia may inadvertently compromise the autonomy of both vulnerable individuals and ordinary members of the community and may further erode the already precarious social bonds that bind communities together and facilitate the integral development of moral agents.
This briefing paper begins by outlining two dominant contemporary perspectives on autonomy – autonomy as informed consent and autonomy as self-definition – and then proceeds to discuss the rhetoric of autonomy in the euthanasia and assisted suicide (EAS) debate. It warns of the disempowering effects that euthanasia can have on vulnerable members of the community. This briefing concludes by outlining an alternative conception of autonomy that addresses the deficits of a liberal individualist conception of autonomy. Paradoxically, if we wish to enable true autonomy at the end of life, we ought to place reasonable constraints on one's ability to actively end one’s life.
Much could be said about contemporary conceptions of autonomy, in part because the concept of autonomy is so hotly contested. This section outlines two dominant views of autonomy in bioethics, namely, autonomy as informed consent and autonomy as self-definition.
Philosophers have engaged in extensive debate about the nature of autonomy in recent decades. Communitarian critics of autonomy argue that a liberal conception of autonomy – a view that conceptualises the individual as self-sufficient and existing in isolation from other members of society – ignores the fact that human beings are situated within communities and ought to focus first of all on the ethical norms that arise from one’s membership of communities. [1] Similarly, feminist critics of autonomy argue that liberal political theorists overlook the relational dimensions of autonomy, and, in particular, the fact that autonomy can be enhanced or diminished based on the social conditions and network of relationships in which one is embedded. [2] Yet it would be beyond the scope of this briefing to canvas the variety of perspectives on autonomy that exist in the literature. Suffice it to say that certain philosophical accounts of autonomy influential in the second half of the 20th century – so-called political liberal accounts of autonomy – have come under increasing criticism in recent years. Political liberalism – even if it may be categorised as a ‘progressive’ philosophical doctrine – prioritises the interests of those who are already afforded the most autonomy in society because of their social status and further disenfranchises those who are subject to social disadvantage.
‘Autonomy’ in contemporary medical ethics is often characterised with reference to decisions about medical treatment and participation in medical research, and the principle of respect for autonomy – one of the four principles of biomedical ethics – is defined with respect to the criteria necessary for informed consent. [3] Beauchamp and Childress, for example, define decision-making autonomy in terms of three necessary criteria: intentionality, understanding, and control. [4] In Beauchamp and Childress’s opinion, a medical decision is autonomous if someone makes a fully informed, deliberate and non-coerced choice; anything short of this fails to meet the criteria necessary for informed consent. Contemporary biomedical ethics guidelines use these criteria for consent as the foundation for ethical standards in medical research (see, for example the Australian National Statement on Research Involving Human Participants). [5] Contemporary bioethical debates also often turn on whether limits can be placed on informed consent requirements for medical treatment.
Another common understanding of the term ‘autonomy’ is that of autonomy as self-definition. That is to say, contemporary conceptions of autonomy are often concerned with “the right to define one's own concept of existence, of meaning, of the universe, and of the mystery of human life”. [6] Autonomy, in this sense, is not just about respect for the basic liberties of patients or participants in medical research. Nor is autonomy reducible to some classical liberal principle guaranteeing freedom from state interference or duress from oppressive actors. Rather, autonomy is deployed with reference to the control that moral agents exercise over their own lives and the ability of agents to shape their own sphere of existence in accord with their own conception of the good. [7] Thus we have the emergence of bioethical rights such as ‘reproductive rights’, ‘the right to die’, ‘the right to have a child’ in the context of assisted reproduction, and ‘trans-rights’ in the context of gender affirmation therapies. Autonomy is not just about having the freedom to make major life choices such as what career one will pursue or whether one will get married. Autonomy is also about defining one’s own microcosm of life in accord with the values that one asserts to be important – to the extent that one can redefine what were once thought of as ineradicable realities of the human condition. For example, sex and gender are no longer viewed as immutable characteristics of the person; human reproduction has become a lifestyle choice rather than a biological reality supervening on sexual intercourse; and the taking of one’s own life is no longer a red line that one ought not cross, but rather a reasonable response to irremediable suffering.
With these accounts of autonomy in mind, we can turn to consider the rhetoric of autonomy in the EAS debate. Autonomy – conceived as a broad right to self-definition – functions as a central ethical plank in the public argument for the legalisation of euthanasia. The website of Dignity in Dying UK, for example, contains three slogans that summarise the organisation’s mission, two of which are directly linked to the notion of defining the terms on which one dies. First, the organisation seeks to provide individuals with “CHOICE over where we die, who is present and our treatment options”. The organisation also seeks to provide people with “CONTROL over how we die, our symptoms, pain relief and planning our own death”. [8] On a superficial reading, these slogans pertain to the noble bioethical goal of empowering patients in clinical decision-making at the end of life. Yet the organisation also has in mind giving terminally ill patients the right to actively end their lives at a time of their choosing. That is to say, autonomy in end-of-life choices is not just about what treatments one receives at the end of life; it is also concerned with dying on ‘one’s own terms’ – to the extent that one may ask a physician to deliberately bring about one’s death (euthanasia), or else seek the assistance of a physician who might provide one with the means of bringing about one’s own death (physician assisted suicide). The legalisation of EAS is thus positioned along a continuum of bioethical empowerment whereby individuals are enabled to enact their values at the end of life, unimpeded by oppressive medical or social constraints.
The jurisprudence behind the introduction of EAS laws around the world similarly reflects a preoccupation with removing constraints on one’s capacity for self-determination. For example, in Carter v. Canada, the bench of the Supreme Court of Canada stated that suicide in the context of terminal illness is a manifestation of the liberty and security of the person – basic rights protected under the Canadian Charter of Rights and Freedoms. [9] The justices wrote that:
The law allows people [nearing the end of life] to request palliative sedation, refuse artificial nutrition and hydration, or request the removal of life-sustaining medical equipment, but denies them the right to request a physician’s assistance in dying. This interferes with their ability to make decisions concerning their bodily integrity and medical care and thus trenches on liberty. And, by leaving people like Ms. Taylor to endure intolerable suffering, it impinges on their security of the person. [10]
Liberty is here understood as protecting “the right to make fundamental personal choices free from state interference” whereas security of the person encompasses “a notion of personal autonomy involving […] control over one’s bodily integrity free from state interference”. [11] In other words, one’s life and one’s body ought to be under the dominion of one’s own will rather than constrained by restrictions that the state might put in place, even if these restrictions are for the sake of upholding basic societal values.
The court rejected defence arguments appealing to the ‘right to life’ enshrined in the Charter, arguing that there is nothing problematic about someone choosing to waive their right to life:
[…] we do not agree that the existential formulation of the right to life requires an absolute prohibition on assistance in dying, or that individuals cannot “waive” their right to life. This would create a “duty to live”, rather than a “right to life”, and would call into question the legality of any consent to the withdrawal or refusal of lifesaving or life-sustaining treatment. [12]
A right to life, then, on this view, does not necessarily prohibit rational and considered decisions to hasten or even directly cause one’s own death. One can essentially decide whether and when one avails oneself of basic human rights.
Autonomy in the EAS debate, therefore, is not just an abstract value corresponding to the practice of informed consent. Autonomy is also conceived of as a right to be free from constraints on one’s will and a right to define one’s life (and one’s death) in accord with one’s own conception of the good. Institutions like medicine, furthermore, ought to function as enablers of moral agents’ capacities for self-determination, rather than placing constraints on an agent’s capacity for choice. That is to say, medicine in contemporary liberal societies is expected to function as a tool of self-actualisation for individuals in addition to any other role it may serve in restoring people to health and relieving suffering.
While the rhetoric of choice may sound intuitively appealing to a contemporary audience, there are a number of serious issues that arise when it is proposed that EAS be legalised for terminally ill patients. A preoccupation with autonomous choice at the end of life undermines other ethical values and, ironically, may actually diminish the autonomy of terminally ill patients.
At the most fundamental level, we ought to consider whether there is a moral precept concerning the taking of human life that ought to function as a limiting principle on individual autonomy – a red line that ought not be crossed. There are strong reasons to think that there is. It is a dangerous misrepresentation to say that autonomy overrides the right to life, such that individual agents can choose to “‘waive’ their right to life”. [13] A principle of fundamental human equality, which presupposes the inalienability of the right to life of the human person, is a necessary ethical principle of a civilised society. Aside from ensuring the maintenance of social order, fundamental human equality ensures that members of society who might otherwise be subject to discrimination – people living with disabilities, people with chronic health conditions, older members of the community, and so forth – are treated with dignity rather than derision, and respect rather than repugnance. The treatment of care home residents in the early stages of the COVID-19 pandemic is one example that witnesses to a worrying erosion of the principle of human equality in Western societies. [14] As Charles Camosy warns, “if we continue on our current path […] the idea of fundamental human equality may simply die out”. [15]
The use of a radical conception of autonomy to sanction EAS risks replacing the principle of fundamental human equality with a crude ethics of autonomy. The idea that people can “‘waive’ their right to life” in principle licenses much more than EAS on the grounds of terminal illness. Such a direct challenge to the right to life is, in fact, a gateway to rational suicide independent of one’s state of health, and could lead to a kind of death on demand whereby the only criteria for receiving EAS is an individual’s autonomous will. It would be unjust to say that people can waive the right to life in some circumstances but not others. Either one says that the right to life is inalienable, or one says that it can be alienated by a rational and autonomous subject at any moment. There is no defensible middle ground.
A significant issue in public discourse on autonomy is that commentators ignore the effects that the one moral actor’s autonomous choices can have on other moral actors. The reality is that one agent’s exercise of autonomy can lead to a diminution of the autonomy of other agents. This idea is compellingly explained in the bioethical papers of American philosopher David Velleman. Regardless of the ostensible public support that exists in favour of EAS, there will always be vulnerable members of the community who do not want to have to confront the question of whether they should avail themselves of a legal option to end their own life. Many people may not want to have this choice available, because, in the words of Velleman, “to offer the option of dying may be to give people new reasons for dying”. [16] In a world where so many dwell in a rational space where the value of continued existence is in constant question, the option of EAS could alter the personal existential calculus of vulnerable individuals in catastrophic ways. This is one clear autonomy-based argument against the legalisation of EAS. [17]
Finally, people nearing the end of life often have diminished autonomy and it thus becomes difficult to justify giving terminally ill patients total autonomy to decide whether they will end their own lives. Crucially, agency – understood as the human capacity to freely choose one’s thoughts, motivations and actions without undue internal or external influences – comes apart from a crude conception of autonomy in morally important ways. One can meet Beauchamp and Childress’s criteria for autonomy, namely, intentionality, understanding and control, while still experiencing diminished agency. Factors that diminish agency include a loss of meaning and purpose in life, a bleak and pessimistic outlook on the future and a distorted perception of one’s own prognosis. [18] Indeed, a desire for death or a loss of the will to live would ordinarily be seen as a factor that impairs one’s capacity for rational judgement. Yet in the case of EAS, this sentiment becomes the very context for decision-making. EAS thus distorts conventional conceptions of agency and leads to the adoption of a crude conception of autonomy whereby one only requires the ability to understand information and the absence of overt forms of coercion. This dimension of decision-making about EAS is particularly insidious. EAS challenges the traditional constraints that we put on decision-making in situations of severe depression or demoralisation, leading instead to a scenario in which these factors provide legitimacy and rational justification for one’s decision.
Readers should note that liberal democratic societies already place quite significant limits on the exercise of autonomy (limits that any reasonable person ought to be able to accept). No one argues that the good of autonomy should allow child abuse, for example. Nor do people protest public decency standards or traffic regulations, save for exceptional circumstances. Current social circumstances demonstrate, therefore, that the argument ‘my body my choice’ is crude and not accepted in many spheres outside of healthcare. Indeed, it is not at all clear that it holds in healthcare either, if we consider the strict public health measures that have been introduced across the globe in response to the COVID-19 pandemic. The notion that the logical conclusion of upholding the good of autonomy necessarily means legalising EAS is inherently flawed. Autonomy is a value that is important but also is the subject of appropriate limits that protect the common good.
The excessive emphasis on autonomy in recent decades draws attention to the dangers of conceiving of this value in a moral vacuum. We ought to instead theorise autonomy within the context of other values that are of fundamental social importance. In particular, we ought to acknowledge the symbiotic relationship between autonomy and human dependence, and the role that autonomy plays in the flourishing of human communities. [19]
Autonomy is a portmanteau of two Greek words, namely, αὐτος (autos; ‘self’) and νομος (nomos; ‘law’). Autonomy, thus, is concerned with self-legislation or self-governance. The autonomous individual is one who is capable of moral self-determination and who is free from external and internal constraints on their motivations, thoughts, decisions and actions. The concept need not be cashed out in terms of an atomistic, liberal conception of the self and society. [20] Even on that worldview, one can still argue for limitations on autonomy, such as traffic regulations. Otherwise, one could not drive anywhere for fear of other drivers being on the wrong side of the road. Rather, autonomy can be understood within the context of an integral vision of human communities. Two considerations are particularly relevant here: the role that autonomy plays in the realisation of basic goods; and the role that communities play in facilitating authentic exercises of autonomy.
First, autonomy can be conceived of as part of a matrix of social conditions that taken together are conducive to the realisation of basic human goods. In their recent book The Way of Medicine, Curlin and Tollefsen identify two functions that illustrate the importance of autonomy in human flourishing. [21] First, some goods are only realised if people make commitments (e.g., marriage, friendship, religion). That is to say, some goods come into being via certain commitments made by persons. Marriage, for example, is a contract (or covenant) between two individuals (a man and a woman, on the traditional conception). Second, commitments also help human beings in community to realise goods to a greater degree, in themselves and one another. If society were governed in a totalitarian manner whereby people of working age were merely assigned to professional roles rather than voluntarily choosing to occupy such roles, we would probably end up with a workforce that is less dynamic and cohesive than one which is made up by free actors.
Such a workforce would be less efficacious in their pursuit of the basic goods constitutive of the flourishing of society.
Second, the exercise of authentic autonomy is enabled by virtue of the human communities to which one belongs. Indeed, the self that is at the heart of any plausible conception of autonomy is a self that is shaped and formed through communities such as the family, friendships, neighbourhoods, educational institutions, intellectual communities, clubs and societies, religious tradition(s), and so forth. The circumstances of one’s life can vary remarkably with respect to the communities to which one belongs. Yet one fact is undeniable: from childhood to old age, from times of health to times of illness and disability, human beings are constantly dependent on each other to know themselves and the world and to make decisions that are conducive to their wellbeing. Most relevant for our purposes, an individual’s reliance on the help, support and encouragement of other human beings is typically most acute in one’s final days and hours.
We have observed how, in the context of EAS, autonomy is deployed in a manner that ironically threatens the agency of all members of the community – the vulnerable in particular but also the very individuals who avail themselves of the so-called ‘right to die’. It makes a virtue of factors like severe depression, demoralisation and a sense of abandonment that are typically regarded as psychological states that undermine autonomy. It also gives people a choice that they may not want to have. [22] With this in view, we ought to consider whether EAS is a proposition that will enable true and authentic expressions of autonomy or whether it will in fact undermine the autonomy of both individuals and communities. Aside from eroding a sense of the interconnectedness of humanity, legalised EAS will ironically undermine the community constraints that typically prevent people from using their autonomy in a manner that is not reflective of their true and considered preferences. It furthermore forces vulnerable people to make a choice that they may very well not wish to make.
One challenge is knowing when policies are sufficiently harmful to the common good to be worthy of public prohibition. Certainly some actions, like the kinds of food that someone wants to eat, should not be subject to public regulation. Yet surely there are also some moral constraints that should govern the use of autonomy. Even John Stuart Mill – one of the great proponents of liberal individualism – saw selling oneself into slavery as a limiting principle on autonomy. Acts that harm others are also a limit on autonomy recognised in Mill’s harm principle. [23] What about voluntary euthanasia and assisted suicide? While proponents of EAS have tried to convince society that it is a private act that does not pose a risk to vulnerable members of the community, the evidence presented in this briefing suggests otherwise. [24] Autonomy-based arguments fail to provide support for the legalisation of EAS. On the contrary, we do harm to both individuals and communities if we were to provide state-sanction to suicide at the end of life.
[1] Alasdair MacIntyre. After Virtue: A Study In Moral Theory. South Bend: University of Notre Dame Press, 1981; Michael Sandel. Liberalism and the Limits of Justice. New York: Cambridge University Press, 1982; Charles Taylor. “Atomism”. In Alkis Kontos (ed.). Powers, Possessions and Freedom: Essays in Honour of C.B. Macpherson. Toronto: University of Toronto Press, 1979.
[2] John Christman. “Autonomy in moral and political philosophy”. In Edward N. Zalta (ed.). The Stanford Encyclopaedia of Philosophy (Fall 2020 ed.). Palo Alto: Stanford University Press, 2020. Available from: https://plato.stanford.edu/archives/fall2020/entries/autonomy-moral/
[3] Lisa Dive, Ainsley Newson.
“Reconceptualising autonomy for bioethics”. Kennedy Institute for Ethics Journal 2018 28(2): 171-203.
[4] Tom Beauchamp and James Childress. Principles of Biomedical Ethics. New York: Oxford University Press, 2001: 63-64.
[5] National Statement on Research Involving Human Participants (Australian Government National Health and Medical Research Council), 2007 (updated 2018): https://www.nhmrc.gov.au/about-us/publications/national-statement-ethical-conduct-human-research-2007-updated-2018
[6] Justice Anthony Kennedy. Planned Parenthood of Southeastern Pa. v. Casey (91-744), 505 U.S. 833 (1992).
[7] For a useful discussion of the related notion of expressive individualism, see Carter Snead. What It Means to Be Human: The Case for the Body in Public Bioethics. Cambridge: Harvard University Press, 2020: Ch.2.
[8] See www.dignityindying.org.uk
[9] See Carter v Canada (AG), 2015 SCC 5.
[10] Ibid., 66. ‘Ms. Taylor’ refers to Gloria Taylor, a woman suffering from amyotrophic lateral sclerosis (ALS) who was a party in the Carter v Canada case.
[11] Ibid., 64.
[12] Ibid., 63.
[13] Ibid.
[14] Xavier Symons. COVID-19 Briefing Paper 4: Care Homes and Older Members of the Community. Oxford: Anscombe Bioethics Centre, 2020. Available from: https://bioethics.org.uk/research/covid-19-briefing-papers/care-homes-and-older-members-of-the-community-dr-xavier-symons/
[15] Charles Camosy. Losing Our Dignity: How Secularised Medicine is Undermining Fundamental Human Equality. New York: New York City Press, 2021: 15.
[16] David Velleman. “Against the right to die”. The Journal of Medicine and Philosophy 1992 17(6): 665-681; 676.
[17] Xavier Symons and Reginald Chua. “‘Alive by default’: An exploration of Velleman’s unfair burdens argument against state sanctioned euthanasia”. Bioethics 2019 34(3): 288-294.
[18] George Mendz and David Kissane. “Agency, autonomy and euthanasia”. Journal of Law Medicine and Ethics 2020 48(3): 555-564.
[19] Alasdair MacIntyre. Dependent Rational Animals: Why Human Beings Need the Virtues. Chicago: Open Court, 1999.
[20] Cf. Dive and Newson (2018).
[21] Farr Curlin, Christopher Tollefsen. The Way of Medicine: Ethics and the Healing Profession. South Bend: Notre Dame, 2021.
[22] Cf. MacIntyre (1999); Dive and Newson (2018).
[23] John Stuart Mill. On Liberty. London: John W. Parker and Son, 1869.
[24] See also the other insightful and well-researched briefings in this Anscombe Bioethics Centre series.
Most recent
Suicide Prevention: Does Legalising Assisted Suicide Make Things Better Or Worse? (Professor David Albert Jones)
08 November 2022
Disability and Assisted Suicide: Elucidating Some Key Concerns (Professor Tim Stainton)
28 August 2022
Euthanasia Case Studies from Belgium: Concerns About Legislation and Hope for Palliative Care (Professor Benoit Beuselinck)
13 December 2021
Support Us
The Anscombe Bioethics Centre is supported by the Catholic Church in England and Wales, Scotland, and Ireland, but has also always relied on donations from generous individuals, friends and benefactors.