Voluntary Euthanasia & Physician-assisted Suicide: The Two ‘Slippery Slope’ Arguments* (Professor John Keown)
Read in PDFThe criminal law and professional medical ethics have long held it wrong for physicians intentionally to kill patients who request it (voluntary euthanasia or VE) or to assist them in suicide (physician-assisted suicide or PAS). This is because all patients have lives worth living: whatever their sickness or disability, they share a fundamental dignity and equality, and any suffering warrants care not killing. Some people disagree, thinking that certain patients would be ‘better off dead’. Whichever ethical view one takes, there remain two powerful ‘slippery slope’ arguments – logical and empirical – against legalisation.
Logically, one cannot sensibly limit legalisation to PAS for the ‘terminally ill’. The standard moral justifications for such a law are: (i) respect for patient choice and (ii) the duty to relieve suffering. But those are equally arguments for PAS for the chronically ill.
Moreover, those two arguments are equally a case for VE, especially for those unable to kill themselves even with medical assistance.
Further, acceptance of the moral case for VE commits one to accepting non-voluntary euthanasia or NVE: lethal injections for patients incapable of requesting them. The absence of (i) patient autonomy does not cancel (ii) the duty to relieve suffering.
Finally, as an empirical matter, laws allowing either VE or PAS cannot ensure effective control in practice and prevent abuse and mistake. It is simply not feasible to draft and enforce effective safeguards. This has been amply confirmed by those jurisdictions that have relaxed their laws, most notably the Netherlands and Oregon.
People disagree about whether it is ever ethical in principle for a physician to administer a lethal injection to a competent patient who autonomously requests it to put an end to suffering (voluntary euthanasia or VE), or for a physician to assist a patient to end their life by prescribing a lethal drug (physician-assisted suicide or PAS). [1]
Professional medical ethics and the criminal law have long held that it is always wrong for a physician intentionally to kill a patient or assist a patient in suicide. As the House of Lords Select Committee on Medical Ethics aptly put it in 1994, the legal prohibition on intentional killing is the ‘cornerstone of law and of social relationships’ that ‘protects each one of us impartially, embodying the belief that all are equal’. [2]
Others, by contrast, think that the lives of some patients are no longer worth living, perhaps because of pain, suffering or disability; that they would therefore be ‘better off dead’, and that physicians ought morally to grant their requests for a hastened death.
However, even many people who think that VE and/or PAS are in principle ethical in ‘hard cases’ nevertheless oppose their legalisation. They do so because they consider that legalisation would result in the extension of the practices to cases that are clearly objectionable, such as the administration of lethal injections to incompetent patients (that is, non-voluntary, euthanasia or NVE). In short, they judge, legalisation would propel society down a dangerous ‘slippery slope’. The ‘slippery slope’ argument against legalisation comprises two independent arguments: the ‘logical’ and the ‘empirical’. [3] We will focus on these two arguments as they apply against the legalisation of VE, though we will also mention their force against the legalisation of PAS.
(i) From VE to NVE
The ‘logical’ argument against legalising VE is that, even if precise guidelines could be framed and enforced so as to permit VE only in the sort of ‘hard cases’ on which euthanasia campaigners and the media focus, where it is freely requested by competent patients in cases of ‘terminal illness’, the moral case for euthanasia with those limitations is also, logically, a case for euthanasia without them. [4]
If euthanasia is justified to end the suffering of a competent patient, why not of an incompetent patient? If euthanasia is justified to end the suffering of the terminally ill, why not of those with chronic illness, whether physical or mental?
Let us consider first the logical link between VE and NVE. Acceptance of VE requires acceptance of NVE because the former rests fundamentally on the judgment that patients who merit VE would be ‘better off dead’, which judgment can logically be made even if the patient, such as an infant or a person with advanced dementia, is incapable of making an autonomous request for death.
The proposals typically advanced by advocates of VE and PAS have long envisaged a central role for doctors not only in the termination of life itself but also in the decision to terminate life. They are not proposals for euthanasia on demand, that is, simply at the patient’s request and without the considered judgment and approval of a responsible doctor. In other words, the case for VE made by its own proponents rests not only on respect for the patient’s autonomous request but also on the principle of beneficence.
A doctor is thought to be justified in ending the patient’s life because in certain circumstances, like ‘terminal illness’, death is thought to be a benefit to the patient, a benefit that it is the doctor’s duty to confer. Doctors are not robots who mindlessly comply with their patients’ wishes, whether for antibiotics or surgery. They are professionals who form their own judgment about the merits of any request for medical intervention. A responsible doctor would no more agree to kill a patient merely because the patient autonomously requested it than the doctor would prescribe antibiotics or amputate limbs. The doctor, if acting professionally, would decide in each case whether the intervention would truly benefit the patient; whether, in the case of a request for euthanasia, the patient would, in the doctor’s judgment, be ‘better off dead’.
Consequently, the underlying, rather than the superficial, justification for VE is not so much the patient’s autonomous request as the doctor’s judgment that the request should be granted because death would benefit the patient. True, in the proposals advanced by VE campaigners, this judgment would not be made without an autonomous request by the patient. But even under such proposals the autonomous request is not decisive. The request serves to trigger the doctor’s judgment about the merits of the request. The doctor decides whether or not the patient would be ‘better off dead’. The patient proposes but the doctor disposes. And, if a doctor can make this judgment in relation to an autonomous patient a doctor can, logically, make it in relation to an incompetent patient.
To put it another way, VE is said to be justified by respect for patient autonomy and by the duty of beneficence, but the absence of autonomy does not cancel the duty of beneficence.
The doctor who performs VE may claim it is justified by respect for the patient’s autonomy and by the duty of beneficence. The doctor who performs NVE cannot rely on respect for autonomy but can invoke the duty of beneficence. If euthanasia were to be made available to suffering competent people who requested it, why would it not be unjustly discriminatory to deny the benefit of a hastened death to those who were suffering but incompetent to request it? Most (and very possibly all) of the leading philosophers who advocate VE also, logically, endorse NVE.
Logic also questions two other limitations common to proposals for legal reform: the limitation of VE or PAS to ‘terminal illness’ and the limitation to PAS.
(ii) From Terminal Illness to Chronic Illness
The argument for VE or PAS for the terminally ill is typically couched in terms of the doctor’s duty of beneficence, the duty to alleviate the patient’s suffering. Why, it is asked, should the terminally ill be allowed to suffer when there is the alternative of a hastened death? However, if it is ethical to end the life of a terminally ill patient to end their suffering, it is also ethical to end the life of a chronically ill patient to end their suffering. Indeed, the argument for intervention is even stronger for the patient with a chronic illness, whether physical or mental, who will not only have longer to suffer but who may be suffering more gravely.
(iii) From PAS to VE
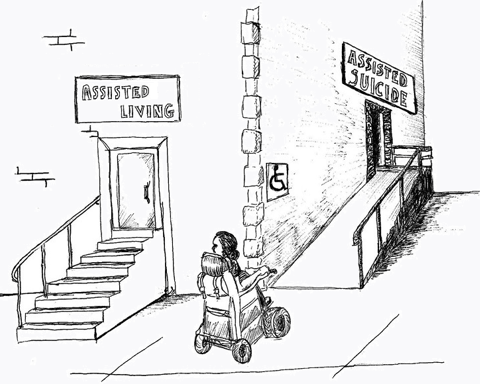
Proposals for legalisation in the US and the UK are typically limited to PAS. But it makes no more moral sense to limit a hastened death to this method than it does to limit a hastened death to the competent or to the terminally ill. If the moral justification for PAS is respect for the autonomy of those who request it, and the physician’s duty to alleviate suffering, those arguments equally justify VE.
Moreover, what if a patient is physically unable to end their own life, even if a physician provides them with a prescription for a lethal drug, perhaps because the patient is totally paralysed? Why should that patient be denied the benefit of a hastened death? Is that not unjust discrimination against those with such a disability? Or what if the patient is old and frail, fears botching their own suicide and would much prefer the physician to administer a lethal injection? Why should their preference be denied? Jurisdictions beyond the US that have relaxed their laws, such as the Netherlands and Canada, appreciate that allowing only PAS is morally unjustifiable.
(iv) An Explanation for the Limitations
Why, then, given that the limitations to competent patients; to terminal illness, and to PAS make little moral sense, do we find them in proposals for reform in the US and the UK? One obvious answer has more to do with politics than ethics: it is more feasible to garner popular and legislative support for proposals that are limited in such ways. The limitations may serve to assuage some peoples’ fears about a likely descent down the slippery slope. One leading US campaigner, Booth Gardner, former governor of Washington State, explained that although he supported a proposal to allow PAS for the ‘terminally ill’, he wanted a wider law. He saw his campaign as ‘a first step’. If he could persuade his state to adopt a limited law then other states would follow and gradually ‘the nation’s resistance will subside, the culture will shift and laws with more latitude will be passed’. [5]
Another leading advocate of relaxed laws, discussing the ‘next generation’ of such laws, has described the limitations in the US laws allowing PAS as ‘burdensome obstacles’. [6] He has criticised the laws’ exclusion of VE; of patients with six months to live; of mature minors, and of advance requests. His criticisms hit the mark. What logical justification is there for any such limitations? There can be little doubt that, sooner or later, whether as a result of legislative or judicial challenge, these limitations will be consigned to history.
(i) The Empirical Argument
The empirical argument is distinct from the logical argument but complements it. It holds that even if a line could be drawn in principle and between VE in ‘hard cases’ and less hard cases, a slide will inevitably or at least very likely occur in practice because the safeguards to prevent it cannot be made effective. Even as a purely practical matter, VE resists effective regulation.
Any attempt at effective legal regulation of VE will be frustrated because of the difficulty if not impossibility of drafting precise guidelines and of then policing them. What, precisely, is meant by a ‘voluntary’ and ‘informed’ request for a lethal injection? And by ‘unbearable suffering’ or ‘terminal illness’? Moreover, even if precise guidelines could be drafted, how could they be enforced? Laws enacted hitherto, such as those in the Netherlands and Oregon, rely largely on self-reporting by physicians after the event. As one leading euthanasia advocate has admitted, this is like enforcing the speed limit by relying on drivers to report their own infractions.
(ii) The Social Background
As a backdrop, we should bear in mind the manifold failings in modern healthcare even in developed countries, where problems of funding and staffing levels often result in overstressed or overtired professionals having to meet unforgiving targets and overstretched budgets. [7] Doctors and nurses often have far too little time to attend adequately to their patients’ needs. There are also grave and growing problems in the provision of adequate social care. The crisis in health and social care seems likely to be aggravated by increasing costs and the growing number of elderly, many of whom have dementia and multiple conditions. The pandemic has served to highlight the grave inadequacies in social and medical care of the elderly and disabled. [8]
Why would these very real pressures not influence patients’ decisions to request VE or PAS as well as the quality of the assessment such requests? Why would deficiencies which currently affect, say, the assessment of patients’ palliative care or mental health needs not also affect assessments for VE or PAS (and many applicants would have unmet palliative care and mental health needs)?
Three particular concerns, which overlap, include capacity, depression, and vulnerability.
(iii) Capacity; Depression; Vulnerability
Capacity. Charland et al have argued that lawmakers and academics have in general failed adequately to point out the practical and ethical challenges embedded in the question when a person has the mental capacity to choose and consent to VE and PAS. The determination of decision-making capacity is a matter of considerable controversy among researchers and clinicians. [9]
Depression. Some of the difficulties facing physicians assessing requests for VE were highlighted by the Royal College of Psychiatrists in 2006 in a Statement responding to a bill to legalise PAS. [10] The Statement noted that studies of the terminally ill had clearly shown that depression was strongly associated with a desire for a hastened death, including PAS, and that once depression was effectively treated almost all patients changed their mind about wanting to die.
It also cautioned that many doctors did not recognise depression or know how to assess for its presence in the terminally ill and that, even when it was recognised, doctors often took the view that understandable depression could not be treated, did not count or was in some way not real depression. [11]
Vulnerability. Baroness O’Neill has voiced concerns about those who are dependent and vulnerable: ‘Legalising “assisted dying” places a huge burden on the vulnerable, let alone the vulnerable and depressed…. Laws are written for all of us in all situations – not just for the unusually independent’. [12]
Legalisation would, moreover, have profound socio-cultural consequences, aggravating vulnerabilities. As one scholar put it, relatives and friends may come to see PAS not only as an acceptable but as a preferred or praiseworthy form of death, and ‘strong social expectations are likely to develop for individuals to choose assisted suicide as soon as their physical capacities decline to a point where they become extremely dependent upon others in an expensive, inconvenient way’. [13] If VE and PAS were available, why should people not be expected to ‘do the decent thing’ and access them, particularly to save resources for their families and the health service?
(iv) Strict Safeguards?
Could the above concerns not be met by ‘strict safeguards’? There is little reason to believe so. It is often claimed that the laws in the Netherlands or Oregon provide examples of laws that have worked well and prevented mistake and abuse, but such claims are very wide of the mark.
Further, Dr Neil Gorsuch (now Justice Gorsuch of the US Supreme Court) has noted that there are many unanswered questions about the Oregon experience (such as the extent to which alternative options, including treatment for depression, are being presented to patients) and that there is little chance of those questions – questions essential to an assessment of the law – being answered any time soon, given the many limitations the law placed on the Oregon Health Authority. [14] Nor is the sparse data reported by that body reassuring. The more recent figures, for 2020, disclose that for over 90% of patients accessing PAS the two main reasons were not pain or suffering but ‘losing autonomy’ and being ‘less able to engage in activities making life enjoyable’; that for more than half a reason was feeling a burden on family, friends and caregivers; and that only 1.2% were referred for psychological evaluation. [15] Moreover, one study indicated that a significant proportion of patients who accessed PAS in Oregon had undiagnosed depression. [16]
As for the Netherlands where, unlike Oregon, comprehensive official surveys of medical decision-making at the end of life have been carried out, those surveys have shown that since the Supreme Court declared VE and PAS lawful in 1984, doctors have, in violation of key legal ‘safeguards’, failed to report thousands of cases to the authorities and have given lethal injections to thousands of patients without an explicit request. Referrals to prosecutors by the review committees for breach of the law have been rare, and prosecutions rarer still. [17]
In short, the guidelines have been consistently and widely flouted, and with virtual impunity. Moreover, Professor Theo Boer, a former review committee member, has lamented the rising incidence of VE and PAS in his country; the expanding interpretation of the guidelines, and the fact that supply has fuelled demand. He has noted the ‘normalisation’ of VE and PAS: they are now increasingly seen not as a last resort but as a normal death. [18]
It is sometimes proposed that abuse or mistake would be prevented by requiring each application for VE or PAS to be approved in advance by a senior judge. This was considered by Lord Sumption in the Nicklinson case, in which the UK Supreme Court rejected a right to VE. Lord Sumption highlighted the risk of pressure, both external and internal, on the vulnerable. He concluded that a court might simply interpose an expensive and time-consuming procedure without addressing the fundamental difficulty, namely, that the wishes expressed by a patient in the course of legal proceedings could be as much influenced by covert social pressures as the same wishes expressed to health professionals or family. [19]
The logical and the empirical arguments against permitting VE and/or PAS are formidable. The logical argument is unanswerable: the moral case for VE is equally a case for NVE, and the case for PAS for the terminally ill is equally a case for VE for the chronically ill.
The empirical argument has yet to be answered, not least by any jurisdiction that has permitted either practice. Indeed, laws such as those in Oregon and the Netherlands serve to illustrate its force, not least because they rely largely on self-reporting after the fact by physicians. The safeguards in the Oregon law are ‘largely illusory’, incapable of detecting mistake and abuse. Claims that it is effectively doing so, and that there has been no abuse, are little more than assertion. Absence of evidence of abuse is not evidence of absence of abuse. Moreover, the logical extension of laws like those in Oregon, involving the removal of its current ‘obstacles’ to wider access, is only a matter of time.
The Dutch experience illustrates the force of both the empirical and the logical arguments. Not only have the guidelines been consistently breached on a wide scale, with virtual impunity, but in 1996 the Dutch courts extended the law to permit NVE, in the form of lethal injections for disabled infants. And in 2016 the government proposed to extend the law to allow healthy elderly folk who feel their life is ‘completed’ obtain assisted suicide.
In short, the slippery slope, both logical and empirical, is very real.
* (Original Paper Published October 2021; Minor Revision, January 2022)
[1] For more on definitions see David Albert Jones, Defining the terms of the debate: Euthanasia and euphemism, (Anscombe Bioethics Centre, 2021).
[2] Report of the House of Lords Select Committee on Medical Ethics HL Paper 21-I of 1993-94 (HMSO, 1994), para 237.
[3] See generally John Keown, Euthanasia, Ethics and Public Policy (Cambridge University Press, 2nd ed, 2018), chapter 6.
[4] See ibid.; see also Daniel Callahan, ‘When Self-Determination Runs Amok’ (1992) 22(2) Hastings Cent Rep 52; Hon Neil M Gorsuch, ‘A Reply to Raymond Tallis on the Legalization of Assisted Suicide and Euthanasia’ (2007) 28 J Leg Meg 327.
[5] Daniel Bergner, ‘Death in the Family’ New York Times Magazine, 2 December 2007.
[6] Thaddeus Mason Pope, ‘Medical Aid in Dying: When Legal Safeguards Become Burdensome Obstacles’ The Asco Post, 25 December 2017. https://ascopost.com/issues/december-25-2017/medical-aid-in-dying-when-legal-safeguards-become-burdensome-obstacles/
[7] It was reported, even before the Covid-19 pandemic, that the complex patchwork of health and social care was straining at the seams. Care Quality Commission, The state of health care and adult social care in England 2016/17 (2017) 4.
[8] See eg: ‘Prejudice against vulnerable patients cannot be allowed to endure’ Daily Telegraph, 10 June 2021. https://www.telegraph.co.uk/opinion/2021/06/10/prejudice-against-vulnerable-patients-cannot-allowed-endure/
[9] Louis C. Charland et al, ‘Decision-Making Capacity to Consent to Medical Assistance in Dying for Persons with Mental Disorders’ (2016) J Ethics Mental Health 1, 3.
[10] Royal College of Psychiatrists, Statement from the Royal College of Psychiatrists on Physician-Assisted Suicide (2006).
[11] Ibid., para 2.4. See also Annabel Price and Simon Wessely, ‘Assisted Dying for the Terminally Ill: The Debate Continues’, Royal College of Psychiatrists, President’s Blog, September 2014. http://bit.ly/2jMcWJX (last accessed 12 January 2018).
[12] Baroness O’Neill of Bengarve, ‘A Note on Autonomy and Assisted Dying’: a memorandum circulated to members of the House of Lords during their consideration of Lord Joffe’s Assisted Dying for the Terminally Ill Bill (2006).
[13] Patricia S Mann, ‘Meanings of Death’ in Margaret P Battin et al (eds), Physician-Assisted Suicide: Expanding the Debate (Routledge, 1998) 11, 21-25.
[14] Neil M Gorsuch, The Future of Assisted Suicide and Euthanasia (Princeton University Press, 2006) 223.
[15] Oregon Health Authority, Public Health Division, Oregon Death with Dignity Act 2020 Data Summary, Table 1. https://www.oregon.gov/oha/PH/PROVIDERPARTNERRESOURCES/EVALUATIONRESEARCH/DEATHWITHDIGNITYACT/Documents/year23.pdf
[16] Linda Ganzini et al, ‘Prevalence of depression and anxiety in patients requesting physicians’ aid in dying: cross sectional survey’ (2008) 337 BMJ: a1682.
[17] See generally John Keown, Euthanasia, Ethics and Public Policy (Cambridge University Press, 2nd ed, 2018) Part III.
[18] Ibid., 234-35, citing Theo A Boer, ‘Rushing toward Death?’ Christian Century, 13 April 2016 and Jacob JE Koopman and Theo A Boer, ‘Turning Points in the Conception and Regulation of Physician-Assisted Dying in the Netherlands’ (2016) 129(8) Am J Med 773.
[19] R(Nicklinson) v Ministry of Justice [2014] UKSC 38 at [228].
Most recent
Suicide Prevention: Does Legalising Assisted Suicide Make Things Better Or Worse? (Professor David Albert Jones)
08 November 2022
Disability and Assisted Suicide: Elucidating Some Key Concerns (Professor Tim Stainton)
28 August 2022
The Principle of Autonomy – Does it Support the Legalisation of Euthanasia and Assisted Suicide (Dr Xavier Symons)
08 April 2022
Support Us
The Anscombe Bioethics Centre is supported by the Catholic Church in England and Wales, Scotland, and Ireland, but has also always relied on donations from generous individuals, friends and benefactors.